Diagnosis and Treatment of Pelvic Venous Syndromes
By Robert Kiser, DO, MSPH
Vulvar varicosities are a source of embarrassment and pain for many women but they are often reluctant to discuss their condition or symptoms with their doctors. These varicosities can easily be missed in casual examination, as they are less obvious in the supine position and may not be seen until the patient stands or assumes an upright sitting or squatting position.
When evaluating lower extremity varicose veins, varicosities in the proximal inner thigh should prompt the physician to consider a pudendal origin. The question, ―Do you have any varicose veins of the vulva or labia? should be asked as well as questions about pelvic congestion symptoms. There are a variety of treatments that can help to improve or eliminate these symptoms.
Pelvic Venous Syndromes: Background and Epidemiology
Vulvar varicosities occur in an estimated 4% of women1 and 15.8-23% of those with lower extremity varicose veins. Most occur during pregnancy and resolve within a few months. When they do not resolve they may cause symptoms of pain, itching, burning, dysparunia, and are perceived by some women as a cosmetic nuisance.
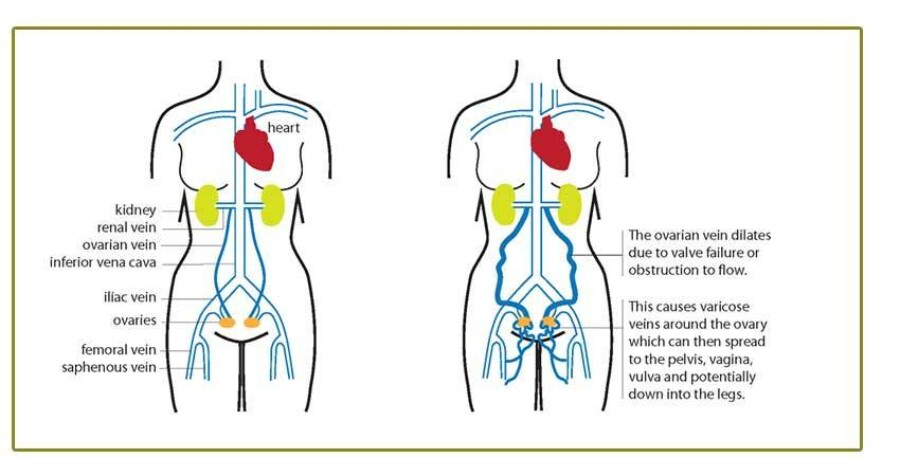
Vulvar varicosities may occur as isolated tributary varicosities or may be a sign of underlying pelvic venous insufficiency. They can also be associated with Pelvic Congestion Syndrome (PCS). PCS results from venous insufficiency (reflux) of the ovarian veins. This important but under-diagnosed condition is associated with symptoms of dysparunia, chronic pelvic pain, feeling of pelvic fullness and discomfort
When signs or symptoms of PCS are reported, a diagnostic transvaginal ultrasound both supine and standing, with and without Valsalva may be ordered to quantify pelvic vein reflux. Magnetic resonance venography is also extremely sensitive to finding dilated gonadal veins and provides an abundance of anatomic information5. Consultation with an interventional radiologist or vascular surgeon for venography and possible coil embolization or fluoroscopy-guided sclerotherapy is warranted when found.
Any patient with symptomatic vulvar varicosities (pregnant or not) should be encouraged to try compression therapy. The company, Prenatal Cradle, makes the V-2 Supporter for the pregnant or non-pregnant woman with vulvar varicosities. This device is similar in appearance to a male athletic supporter, but is contoured to provide compressive support for the vulva, thus preventing the pooling of blood in the labial veins.
Non-surgical and Minimally Invasive Techniques
For vulvar varicosities in the non-pregnant patient, remarkable improvement can be achieved with sclerotherapy. The visible varicosities are injected with a quantity of liquid or foam sclerosant, and the area is then compressed with a pad and the V-2 supporter or similar compression garment7. A few treatments can provide lasting relief and cosmetic improvement in vulvar varicosities. To minimize the risk of complications, the injecting physician should have extensive experience with vein sclerosis and a strong working anatomy of the pelvic venous system.
Persistent Pelvic Congestion Syndrome
For some patients, treatment of vulvar varicosities with a V-2 compression trial followed by compression sclerotherapy affords symptomatic improvement8. Patients with PCS who are not responding to compression should be evaluated by an interventional radiologist or vascular surgeon for possible coil embolization. Under fluoroscopy guidance, the refluxing ovarian veins can be embolized by endovenous insertion of a metallic coil.
After the pelvic venous insufficiency has been treated, if not previously addressed, the vulvar varicosities may be re-evaluated by a phlebologist who practices sclerotherapy to determine whether the varicosities and their associated symptoms have adequately resolved. If not, sclerotherapy of the visible varicosities may be provided if the patient wishes.
Help is available for your patients suffering with Pelvic Venous Syndromes. For more information, call 240-965-3915.