Understanding Post Thrombotic Syndrome
By Gautam Shrikhande, MD
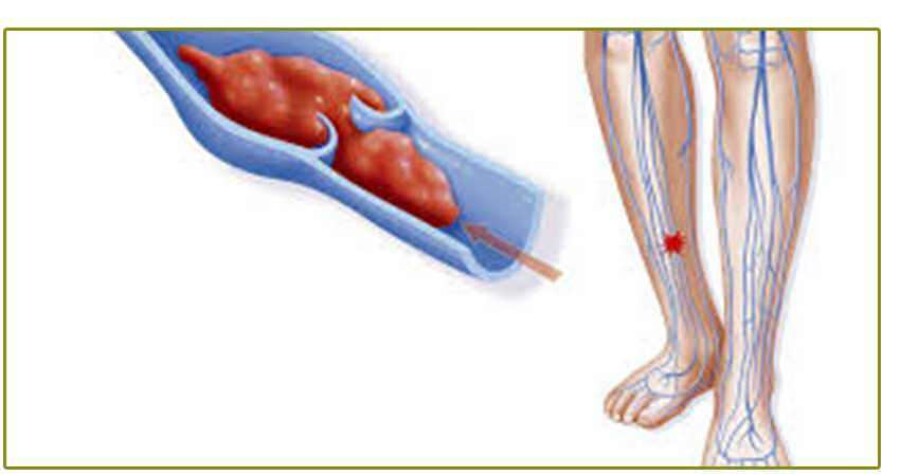
In patients with deep venous thrombosis (DVT), the most significant immediate concern is that of pulmonary embolus. Over the next several months to years, however, development of post thrombotic syndrome (PTS) presents a much more prevalent chronic morbidity. PTS refers to the signs and symptoms that occur as long term consequences of DVT. PTS can affect up to 23-60% of patients in the two years following DVT, and up to 10% of these patients may go on to have ulceration.1 The most significant long term sequelae of PTS are a significant loss of quality of life and limitations in the abilities to perform daily activities.2 Signs and symptoms in the leg include swelling, heaviness, aching, cramping, varicose veins, skin discoloration, and ulceration. The inflammatory response secondary to the thrombus as well as the physical pressure from the thrombus is thought to lead to venous valvular disruption and incompetence. This valvular incompetence combined with persistent venous obstruction from the thrombus increases the pressure in the veins and leads to a state of venous hypertension. Risk factors for the development of PTS include proximal DVT, recurrent ipsilateral DVT, persistent DVT symptoms one month after DVT diagnosis, obesity, and inadequate anticoagulation during the first 3 months of DVT treatment.
The most important initial step in the evaluation of PTS after obtaining a history of DVT is obtaining a venous duplex ultrasound. The key features of this evaluation include the degree of recanalization of the deep venous system, the location of the obstruction (proximal or distal), and the presence of both deep and superficial venous insufficiency.
Understanding Post Thrombotic Syndrome
Initial, conservative treatment options for PTS include appropriate anticoagulation for DVT, leg elevation, weight loss in overweight patients, and the use of elastic compression stockings for up to 2 years post DVT.4 In patients with ulceration development, appropriate wound care and compression bandages are indicated. Also, in some patients, venous ablation in patients with significant superficial venous reflux may provide symptomatic relief.
In addition, from the American College of Chest Physician Evidence-Based Clinical Practice Guidelines in 2012, there is evidence to suggest that catheter directed thrombolysis (CDT) in the setting of acute DVT may reduce PTS and improve quality of life without being associated with an unacceptable increase in bleeding. The patients who experience the best results are those who have ileofemoral DVT for less than 14 days.5 CDT involves taking the patient to an angiography suite and infusing thrombolytic therapy, typically tissue plasminogen activator (TPA), directly into the thrombus. The dissolution of thrombus can prevent the subsequent inflammation of obstruction which occurs secondary to the thrombus and can preserve long term deep venous function.
Lastly, in patients with established PTS, some have shown that venous balloon dilation and stent therapy can be effective treatments for chronic ileofemoral thrombosis.6 With this minimally invasive approach which can be safely and easily accomplished in an angiography suite, patients with PTS can get quick symptomatic relief with minimal morbidity and good patency of the venous system after stenting. We have had several patients with ulcerations in the setting of PTS who have gone onto complete resolution of this pathology.
In summary, PTS can be a significant source of morbidity in patient with DVT, however with the proper evaluation and treatment selection by a venous specialist, PTS can be either prevented or treated to provide patients with an excellent quality of life.