Recent Articles About Vein Health

Treatment Options for Varicose Veins at Any Age
Varicose veins are a common condition that can affect people of all ages, and modern minimally invasive treatment options are safe and effective for older adults. In this blog, a CVR vein physician, Dr. Deborah Cogan, outlines why seeking evaluation and treatment from a vein expert can help address varicose veins, regardless of a person's age, enabling adults of any age to stay active and enjoy their life to the fullest.
What is a DVT Blood Clot in The Leg?
Discover insights into blood clots and their risks in our latest blog by vein specialist Mohamed T. Hassan, MD, DABVLM, RPVI. Delve into the complexities of deep vein thrombosis (DVT), as expertly explained by Dr. Hassan, lead vein specialist at Center for Vein Restoration (CVR). Learn about the types of blood clots, their diagnosis, risk factors, complications, treatment options, and prevention strategies. Empower yourself with the knowledge to safeguard your vascular health and explore our comprehensive vein care services at CVR.
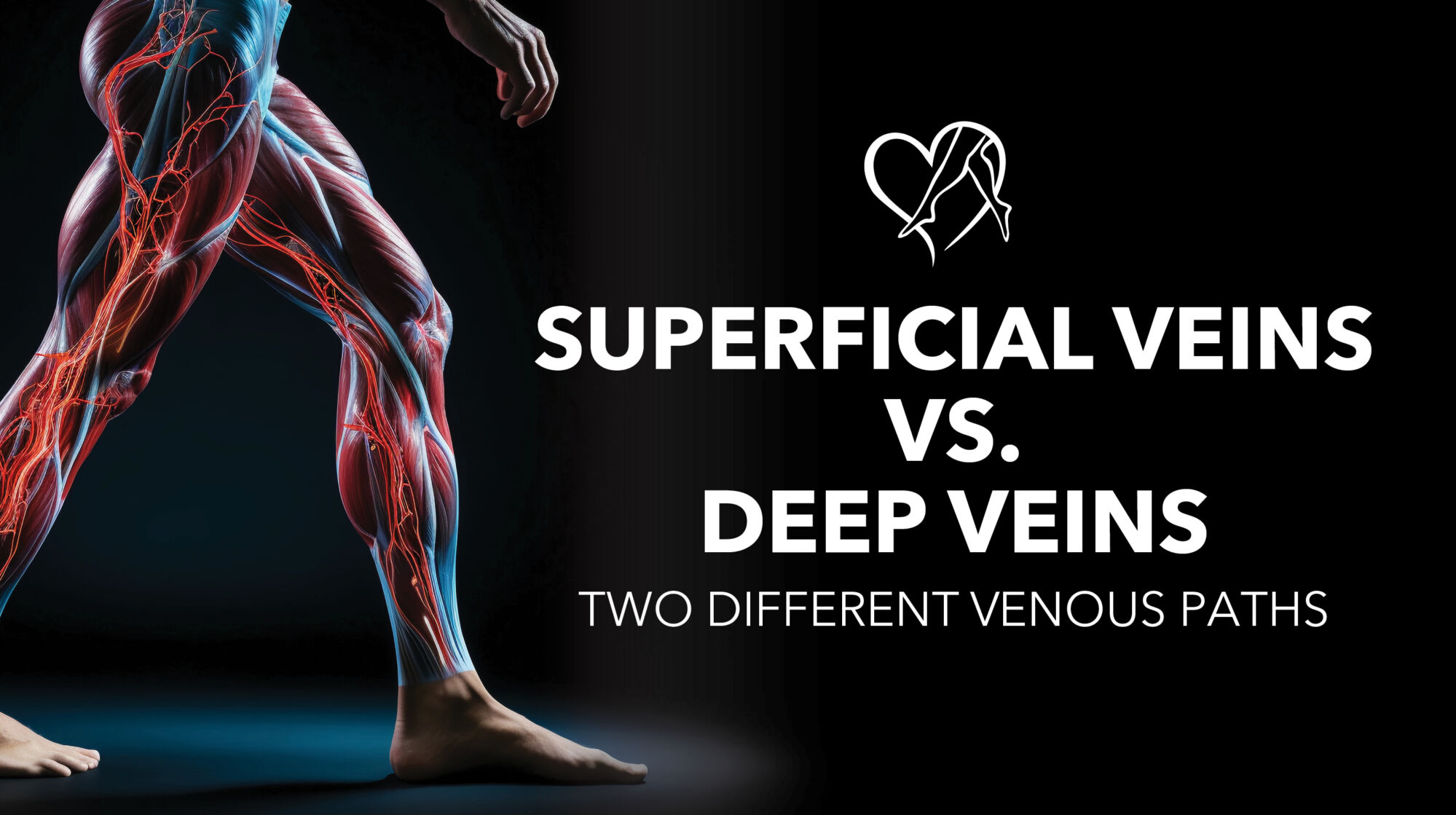
How to Avoid Varicose Veins
In this blog, we will review the causes and risk factors associated with chronic venous insufficiency (the root cause of varicose veins) and offer tips on how to avoid vein conditions. Because several risk factors (such as sex, age, and family history) are out of one's control, we will also provide information about safe and effective outpatient treatment options for people with vein problems.

Are You Getting Aching Legs at Night? Here are Nine Causes of Lower Leg Pain
Explore the nine common causes of lower leg pain, from muscle strains to varicose veins, in this informative guide.

Can You Feel a Blood Clot Move?
The blog delves into the complexities of blood clot formation, their potential risks, and how they can go unnoticed. Highlighting conditions like deep vein thrombosis (DVT) and pulmonary embolism (PE), the blog stresses the importance of recognizing symptoms and seeking prompt medical attention for potentially life-threatening situations. Additionally, it emphasizes the connection between varicose veins and clotting risk, offering resources for diagnosis and management through Center for Vein Restoration, with vein clinics throughout the United States.

How Do You Get Rid of Edema in Your Legs?
If you have edema in your legs, ankles, or feet, reach out to our expert vein specialist for treatment, or learn how to alleviate leg edema effectively with expert tips on elevation, compression, hydration, and medical guidance for severe cases.

Do Spider Veins Mean Blood Clots?
Spider veins are usually harmless and don't indicate blood clots. Consult a vein specialist for accurate diagnosis and appropriate treatment.

How Do You Treat Varicose Veins In The Legs?
Learn about effective treatments for varicose veins in the legs, including lifestyle changes, compression stockings, sclerotherapy, laser therapy, and surgery.