
If you have venous insufficiency (vein disease), you understand the leg pain, swelling, aching, cramping, feelings of heaviness, and telltale twisted or bulging purple or blue leg veins. If you’ve been living with untreated vein disease long enough, you may have developed complications such as skin discoloration, leg ulcers, or a blood clot in the leg.
Click below to learn what varicose veins are, what causes varicose veins, the risk factors, the symptoms to look out for, and the treatment options for varicose veins.
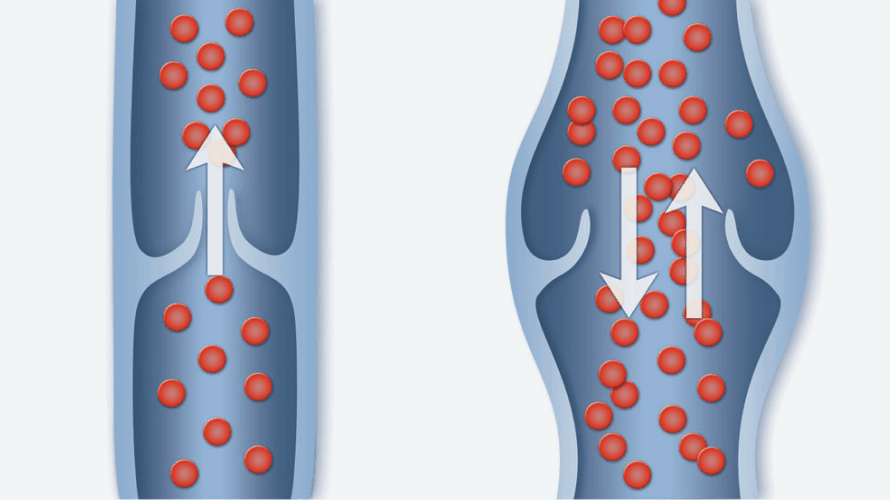
Varicose veins are enlarged, twisted veins that commonly occur in the legs and feet. They develop when tiny valves within the veins don’t work as they should, causing blood to flow backward and pool in the lower limbs. This increases pressure in the veins, causing leg veins to swell and stretch. The increased pressure results in fluid in the leg, which causes heaviness, a constant dull ache, leg fatigue, cramps, and itchiness. If the pressure becomes too great, blood can leak into the skin, causing the skin to turn brownish-black.
Over time, problem blood circulation in the leg veins causes the skin to lose suppleness and flexibility, and skin can gradually take on a hardened texture. In some advanced cases, the skin can rupture, causing an open sore, known as a venous ulcer or venous stasis ulcer, to form. Venous ulcers affect approximately 4 percent of Americans aged 65 and over.
Each year, the complications that result from chronic venous insufficiency (CVI) contribute to the loss of over one million workdays in the United States.
Between 20-30 million Americans have varicose veins. Risk factors include heredity, gender, age, weight, pregnancy, history of deep vein thrombosis (DVT and blood clots), and standing or sitting for prolonged periods. By age 50, 41 percent of women will suffer from varicose veins. By the time they reach their 60s, 42 percent of men will suffer from symptoms related to venous insufficiency.
To diagnose varicose veins, your vein physician will review your medical history for classic venous insufficiency symptoms and conduct a physical examination to assess the location and severity of your condition. A crucial part of the evaluation involves performing a venous ultrasound, which evaluates the functioning of the veins. During the ultrasound, your healthcare team, including the vascular technologist and your vein physician, will specifically look for indications of reflux (blood flowing in the wrong direction). They will also examine for any signs of blood clots or lingering damage from previous clots.
Some veins are difficult to examine with a simple physical or with ultrasonography, specifically veins in your abdomen and pelvis. Those may very well require a more sophisticated examination like a CT scan or MRI. In some cases, an invasive test called a venogram is needed. During the venogram, your doctor injects a special dye into your legs, and X-rays are taken of the area. This test provides your doctor with a more detailed landscape of how and where your blood is flowing and whether or not there are any blockages to blood flow that can be corrected.

A type of vascular ultrasound is done to check blood flow and the structure of the leg veins.
A procedure similar to duplex ultrasound uses color to show the direction of blood flow.
A diagnostic procedure that uses a combination of large magnets and a computer to view the veins. Dye is injected into the veins to see them better. An MRV can also help diagnose other causes of leg pain.
Another diagnostic imaging tool uses an X-ray and a computer to create images of your body.