Diagnosis and Treatment of Pelvic Venous Syndromes
By Robert Kiser, DO, MSPH Vulvar varicosities are a source of embarrassment and pain for many women but they are often

Medically reviewed by Priya Thirumlai, MD, FACS, FACOG, on September 30, 2025
Chronic pelvic pain doesn’t have to control your life, and understanding the cause is the first step toward taking it back—fully and pain-free. Chances are that the pelvic pain you’ve been living with has a name, an origin, and most importantly, a solution.
We consulted with Center for Vein Restoration pelvic and lower leg vein specialist Dr. Priya Thirumlai about pelvic congestion syndrome (PCS), also known as pelvic venous insufficiency. This condition affects up to 30 percent of women who have chronic pelvic pain, according to the National Library of Medicine (NIH). Further, pelvic congestion syndrome is estimated to be present in up to 75.5 percent of patients with pelvic varicose veins, according to a 10-year retrospective analysis reported by the NIH.

Dr. Thirumlai is board-certified by the American College of Obstetrics and Gynecology and is the lead physician at Center for Vein Restoration vein clinics in Alexandria, Virginia, and Easton, Maryland.
📍 To schedule an appointment with Dr. Thirumlai in Alexandria, VA, CLICK HERE.
📌To schedule an appointment with Dr. Thirumlai in Easton, MD, CLICK HERE.
📞To schedule an appointment with Dr. Thirumlai by phone, call 240-965-3915 or CLICK HERE to be connected with a Patient Services Representative.
🚩To schedule an appointment at any of CVR’s 120+ vein clinics nationwide, or click below ⬇️

Chronic pelvic pain (CPP) is a persistent, non-cyclic pain in the lower abdomen and pelvis that lasts for six months or longer. It affects millions of people, primarily women, and can significantly impact quality of life. The pain can be constant or intermittent and is often described as a dull ache, a sharp or stabbing pain, or a feeling of heaviness or pressure.
Doctors don’t fully understand why PCS happens, but researchers point to several likely causes:
The causes of chronic pelvic pain are diverse and can involve multiple body systems. It can be a symptom of a specific disease, such as endometriosis or interstitial cystitis, or it can be a condition in its own right. One of the less-known but significant causes of CPP, particularly in women, is pelvic congestion syndrome, which is often related to a broader vascular condition known as May-Thurner (PCS).
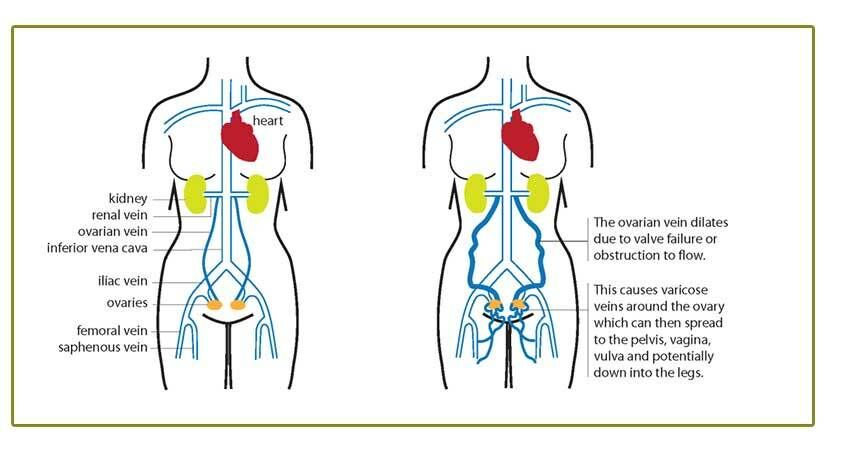
May-Thurner syndrome (PCS), also known as iliac vein compression syndrome, is a vascular condition where an iliac artery compresses the iliac vein against the lumbar spine. While the right iliac artery crossing over and compressing the left iliac vein is the most common cause, compression can also be seen with the left iliac artery, leading to symptoms in either the right, left, or both legs.
The constant pressure from the artery can cause the vein to narrow, leading to the formation of scar tissue and fibrous bands that further restrict blood flow. This causes blood to back up in the affected leg(s) and pelvic veins, leading to various symptoms and complications.
According to Cedars Sinai, PCS mostly presents in women of childbearing age and is more common among women who have had more than one childbirth. Women who have had three or more pregnancies are particularly susceptible due to the weight of the gravid uterus, hormonal changes, and a dip in the pelvic floor, all of which can increase pressure on the iliac veins.
Many individuals with the anatomical variation of May-Thurner syndrome are asymptomatic (meaning no symptoms). When symptoms do occur, they are typically a result of the slowed blood flow and increased pressure in the affected leg(s) and pelvis. The most common symptoms include:
In some cases, the chronic venous pressure and inflammation can cause pain that extends beyond the typical symptoms. While not as common, some patients with May-Thurner syndrome (PCS) may experience:
Although the symptoms are real and can be debilitating, because of its location and the rarity of the diagnosis, May-Thurner syndrome (PCS) can be missed by primary care physicians, gynecologists, and other specialists. This often leads to a long and frustrating journey for patients seeking an accurate diagnosis.

Pelvic Congestion Syndrome and chronic venous insufficiency can be frustrating and isolating—but you’re not alone! CVR is America’s largest physician-led vein center, with 80+ experienced physicians dedicated to helping patients just like you. Our 98 percent patient satisfaction rating speaks to the compassionate care we provide every day.
📍Find a CVR clinic near you and take control of your health and your future.
Diagnosing MTS (PCS) can be challenging due to the varied and sometimes vague nature of the symptoms. A doctor will typically begin with a physical exam and a review of medical history. Imaging tests are then used to confirm the diagnosis and rule out other conditions. These may include:
The primary goal of treatment for May-Thurner syndrome (PCS) is to relieve the compression, restore normal blood flow, and prevent serious complications like DVT.
Common treatment options include:
Because there is increased pressure in the pelvic veins that can be felt in the legs, a complete management plan for May-Thurner syndrome (PCS) often includes venous mapping to look for venous insufficiency in the lower legs. This can help identify if blood is pooling in the legs due to faulty valves in addition to the main compression, allowing for a more complete treatment strategy.
Getting the correct diagnosis is crucial because getting the proper treatment depends on it. Pelvic pain can be multifactorial as well (that is, it can have more than one cause). For example, hip arthritis and pelvic congestion syndrome (PCS) can occur together. If only one problem is treated, it may only provide partial relief, as the other condition continues to contribute to the pain.
👉 Book your consultation with a CVR vein specialist today and discover how simple relief can be.
You don’t have to live with chronic pelvic pain or vein problems any longer. At Center for Vein Restoration (CVR), our compassionate, board-certified vein specialists are ready to listen, diagnose, and guide you toward lasting relief. With more than 120 locations across 22 states, we make expert vein care convenient and accessible.
We accept most major insurances, including Aetna, Blue Cross/Blue Shield, Cigna, Medicaid, and Medicare.
📞 Call Center for Vein Restoration at 240-965-3915
📅 Or book online HERE
While PCS can’t always be prevented, you can lower your chances or ease symptoms by:
You’re not weak, and this pain is not “just in your head.” PCS is real, and an experienced vein specialist knows how to help. Relief is within reach, and a full life is still ahead. If your pain doesn’t get better, keep asking questions and don’t give up! You deserve care from a vein care professional who sees you, hears you, and helps you heal.