Medically reviewed by Mohammad Khalilullah, MD, DABVLM, on July 17, 2025
Short answer: Your legs are trying to tell you something.
It starts as a whisper first: a dull ache after a long day, a twinge when you climb the stairs. Then it gets louder: swelling, burning, or veins that rise like roadmaps under your skin.
Maybe your legs feel heavy by the end of the day, or there’s a deep ache that shows up after sitting or standing too long. Perhaps it’s the swelling around your ankles or those bulging veins that make you uncomfortable and a little concerned.
Your veins are working overtime, and when they start to struggle, your legs speak up in the only way they know how: aching, swelling, pressure, and fatigue. The more we ignore them, the louder they shout. The good news? You don’t have to live with the pain, and help is available.
To schedule a vein appointment with Dr. Mohammad Khalilullah in Winchester, Virginia, or any of Center For Vein Restoration’s other 115+ vein clinic locations, click below ⬇️

America’s Most Trusted Vein Doctors Are Ready to Help
When it comes to your health, you want more than just a quick fix; you want experienced vein specialists you can trust. At Center for Vein Restoration (CVR), you’re in the hands of the most respected vein experts in the country. Our 80+ board-certified physicians are leaders in their field, contributing to peer-reviewed journals, advancing new treatments, and training the next generation of vein doctors.
Whether you’re dealing with varicose veins, spider veins, or leg pain you can’t explain, there’s no better time to schedule a consultation with CVR, the nation’s #1 physician-led vein center.
📞 Call CVR at 240-249-8250
📅 Or book online HERE
What’s Causing Leg Vein Pain?
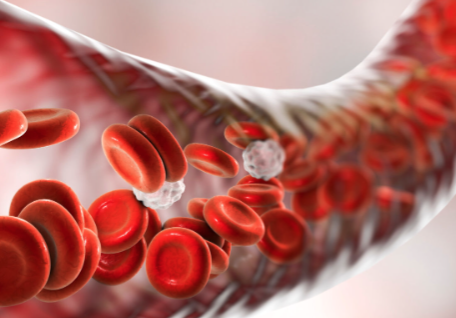
Veins in your legs send blood back to your heart. Tiny one-way valves help push your blood uphill. When those valves weaken or fail, blood can flow backward and pool in the veins. This puts extra pressure on your veins. Called venous insufficiency, this condition causes pain, swelling, heaviness, cramping, and visible changes to the veins.
These stretched veins can be especially tender or achy after being on your feet for extended periods, according to the National Library of Medicine’s MedlinePlus.
Common symptoms include:
- Varicose veins: These are large, twisted, bulging veins that often cause aching, throbbing, heaviness, burning, or cramps.
- Spider veins: Smaller and closer to the skin, usually only cosmetic, but they can hint at bigger problems like venous insufficiency.
- Chronic Venous Insufficiency (CVI): Long-term vein disease where valves in the veins don’t close properly, allowing blood to flow backward and pool in the legs, leading to swelling, pain, varicose veins, itchy skin, and even ulcers.
Could Leg Pain Be Something More Serious?
Sometimes, leg vein pain is a sign of a more serious problem, such as:
- Superficial thrombophlebitis (or superficial phlebitis): Inflammation in veins close to the surface of the skin. According to the Cleveland Clinic, superficial thrombophlebitis is treated using elevation, compression, and nonsteroidal anti-inflammatory drugs. The condition typically resolves in a few weeks
- Deep vein thrombosis (DVT): A blood clot in a deep vein, often the calf or thigh. DVT can be dangerous, even fatal, because the clot can dislodge and travel to the lungs, causing a pulmonary embolism (PE). If you experience sudden swelling in one leg, warmth or redness over a vein, or sharp pain, seek emergency care immediately.
Center for Vein Restoration offers a safe and effective alternative to the ER. Patients can “skip the line” at the ER and receive:
- Same-day evaluation and diagnosis of possible deep vein thrombosis
- Notification of results on the same day
- Immediate start of anticoagulation medication (if indicated)
- Long-term follow-up care until anticoagulation medicine can be stopped
For Center for Restoration DVT rule-out service, call 877-SCAN-DVT (877-722-6388).
Signs You Should See a Vein Doctor About Your Leg Pain
Here’s a quick list of symptoms that mean it’s time to visit a Center for Vein Restoration vein specialist:
- Leg ache or throbbing that lingers
- Swelling or heaviness in your legs or ankles
- Visible varicose veins or spider veins
- Burning, itching, or cramps, especially at night
- Changes in skin color or sores don’t heal. Larger open wounds, itching, or skin thickening might follow
- Warmth, redness, or a lump on a vein, which could be phlebitis or a blood clot
IMPORTANT: Mild symptoms can grow worse if left unchecked. Early diagnosis by a vein expert can help prevent complications such as ulcers or thrombophlebitis.
Call 240-249-8250 to speak with a Patient Services Representative or schedule your consultation online at a CVR near you today.

How Can I Ease Leg Pain at Home?
While heredity and being female (two of the most common risk factors for vein disease) cannot be changed, these simple actions can reduce the risk of vein problems and help alleviate leg pain and swelling:
✅ Stay Active
Exercise helps your leg muscles push blood back toward your heart. Walking, biking, and swimming are great choices.
✅ Elevate Your Legs
Raise your legs above heart level for 15-20 minutes, especially after a day of standing.
✅ Wear Compression Stockings
These special socks apply gentle pressure to your legs, improving blood flow and reducing swelling.
✅ Avoid Long Periods of Sitting or Standing
Take movement breaks every 30–60 minutes if your job or lifestyle involves long periods in one position.
✅ Maintain a Healthy Weight
Extra weight puts more pressure on your veins and can worsen vein disease.
✅ Eat Well & Stay Hydrated
A diet rich in fiber, low in sodium, and high in fruits and vegetables can support better circulation.
What Outpatient Treatments Can a CVR Vein Center Offer?
If self-care isn't enough or if your vein problems are more significant, a Center for Vein Restoration vein doctor can offer minimally invasive, office-based treatments that allow patients to drive themselves to and from the appointment and resume regular activity immediately, with only a few restrictions.
- Sclerotherapy: Injecting a special solution to close off small varicose and spider veins. It even lessens swelling, burning, and aching
- Endovenous laser or radiofrequency ablation: Uses heat energy to seal off larger veins. Quick and done right in an office
- Ambulatory phlebectomy: A Microincision is made to pull bulging veins
- VenaSeal: Proprietary medical adhesive closes off diseased veins
Your Center for Vein Restoration vein specialist will guide you toward the best treatment plan tailored to your needs. These outpatient treatments carry a low risk and allow people to return to their routines immediately.
📞 Call CVR at 240-249-8250
📅 Or book online HERE
Pain Relief Starts with a Conversation
You don’t have to live with leg pain, discomfort, or unsightly veins. At Center for Vein Restoration, we believe every patient deserves personalized, affordable, and state-of-the-art care delivered by people who truly listen.
Your first consultation includes a thorough evaluation, including a painless ultrasound, and a clear plan of action. We’ll even help you get the insurance coverage you're entitled to.
Schedule your consultation with Center for Vein Restoration today and discover the CVR difference—because your legs (and your life!) are worth it.


 About Vein Disease
About Vein Disease
 Spider Veins
Spider Veins
 Varicose Veins
Varicose Veins
 Vein Disease Treatments
Vein Disease Treatments
 Treating Spider Veins
Treating Spider Veins
 Treating Varicose Veins
Treating Varicose Veins
 About Us
About Us
 Patient Resources
Patient Resources
 Physician Resources
Physician Resources



