May-Thurner syndrome is a rare vascular disorder that can put you at risk for a blood clot. But if you’re concerned that it’s a hereditary condition, you don’t have to worry!
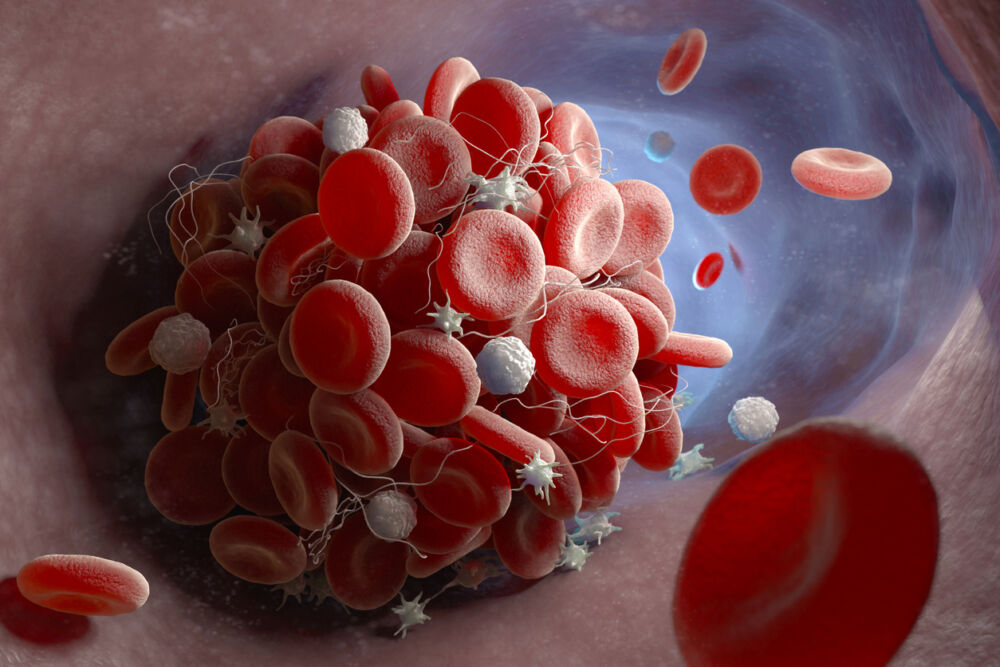
Deep vein thrombosis (DVT), or a blood clot deep in a leg vein, can develop if you sit for long hours on a plane, car, or even at your desk. Having varicose veins also greatly increases the chance of DVT. But did you know that blood clots in the leg can also result from a rare condition known as May-Thurner syndrome?
May-Thurner syndrome affects blood flow in the left leg. Although it is not hereditary, the condition is more common among women who have given birth multiple times or those with a history of blood clots. It’s also believed to be caused by scoliosis and dehydration. Talk to a vascular specialist for diagnosis and treatment if you think you may be at risk of May-Thurner syndrome.
What is May-Thurner syndrome?
May-Thurner syndrome develops due to a malfunction in your circulatory system, specifically between your right iliac artery and your left iliac vein. Your right iliac artery brings oxygenated blood to your lower extremities. Your left iliac vein returns that blood to the heart, where it receives oxygen once again.
Arteries and veins sometimes cross over. But in May-Turner syndrome, the right iliac artery compresses the left iliac vein, interrupting blood flow. When that happens, you may experience pain, swelling, discolored skin, feelings of heaviness, and varicose veins in the left leg.
Many patients with May-Thurner syndrome don’t experience symptoms until a blood clot forms. Extreme swelling, tenderness, and reddish-colored skin are all signs of DVT. These symptoms must be assessed and treated immediately to prevent a life-threatening pulmonary embolism (PE). A PE occurs after the clot lodges in the lungs, causing rapid heartbeat, chest pain, and a bloody cough. If PE symptoms develop, call 240-965-3915 for emergency medical intervention.
Treating May-Thurner syndrome
A vascular specialist can perform an ultrasound, CT scan, or MRI to diagnose May-Thurner syndrome. A venogram can identify compression of the iliac vein via X-ray, allowing your doctor to see the blood flow in your leg veins.
Treatment focuses on improving blood flow and reducing the risk of DVT. It also depends on whether you’ve experienced a DVT due to May-Thurner syndrome. If that’s the case, your doctor may recommend blood thinners, which can dissolve a clot in the vein. Your doctor may also place a vena cava filter in the large vein to stop a clot before it travels to your lungs.
If you have May-Thurner syndrome but haven’t experienced a clot, treatment via several surgical options can lessen the chance of a clot forming. One such method involves inserting a balloon into the left iliac vein. A catheter will inflate the balloon to open the vein, and the doctor will place a stent to ensure uninterrupted blood flow.
Blood can also be rerouted around the compressed vein with a bypass procedure. Tissue from a donor or another part of your body takes the place of the damaged vein, allowing blood to flow smoothly. Another technique is to move the right iliac artery off the left iliac vein by wedging a piece of tissue between the two, lifting the pressure off the vein.
May-Thurner syndrome is difficult to prevent because it has no known cause, it’s difficult to prevent. However, anything you can do to boost circulation will help. Walking and biking promote circulation in the legs, so exercise as often as possible. Managing diabetes, high blood pressure, and peripheral artery disease also help cut the risk of DVT. Stay hydrated and avoid sitting or standing for long periods. Wearing compression stockings is another good way to get the blood moving in your legs.
Take care of your veins!
Healthy veins are vital to overall health, so take care of them! Center for Vein Restoration (CVR) physicians are experienced vascular specialists who can diagnose and treat vein disease, including varicose veins and May-Thurner syndrome.
Contact a CVR office today to schedule an appointment, or call 240-965-3915.

 About Vein Disease
About Vein Disease
 Spider Veins
Spider Veins
 Varicose Veins
Varicose Veins
 Vein Disease Treatments
Vein Disease Treatments
 Treating Spider Veins
Treating Spider Veins
 Treating Varicose Veins
Treating Varicose Veins
 About Us
About Us
 Patient Resources
Patient Resources
 Physician Resources
Physician Resources