
Varicose veins don’t just show up overnight.
Like many health problems, signs and symptoms can follow a slow and predictable path that can be dismissed or shrugged off as “normal.” In the case of venous insufficiency, the root cause of varicose veins and spider veins, the clues often start with harmless-looking surface veins. They can potentially lead to serious skin damage or open ulcers.
That’s why understanding the stages of vein disease can help you take action early, when treatment is easiest and most effective.
Whether you're dealing with mild leg discomfort or swelling, knowing where you fall on the spectrum of venous insufficiency is key to protecting your long-term health. This blog breaks down each stage of varicose veins in clear, simple terms so you can decide when it’s time to see a vein specialist.
From spider veins to open ulcers, every stage of vein disease tells a story, and early action can change the ending. If you’ve noticed discomfort, swelling, or skin changes on your legs, it’s time to get evaluated by a vein specialist. At Center for Vein Restoration, our board-certified doctors use advanced tools and treatments to stop vein disease before it disrupts your life.
Your legs are talking! Listen to them and contact CVR today.
📞 Call CVR at 240-965-3915
📅 Or book online HERE
Inside each leg vein are one-way valves that keep blood moving toward the heart. When these valves weaken or become damaged, blood slips backward and pools in the veins. Doctors refer to this condition as venous insufficiency, which can lead to various vein issues, including varicose veins and spider veins. Over time, the added pressure stretches the vein walls, causing them to bulge, twist, or become visible under the skin.
According to the Mayo Clinic Health System, the effects of gravity, combined with prolonged standing or sitting, make the veins in the legs especially vulnerable, explaining why varicose veins are so common in the lower body. Without treatment, this condition can worsen, increasing the risk of swelling, skin damage, and leg ulcers.
That heaviness, swelling, or skin discoloration in your legs isn’t just a sign of aging—it could be your body’s way of warning you about vein disease. Varicose veins progress over time, and waiting too long can lead to painful ulcers and long-term damage. At Center for Vein Restoration, our expert team is here to diagnose and treat your vein problems before they advance to a more serious stage. Don’t ignore the signs—take the first step toward relief today.
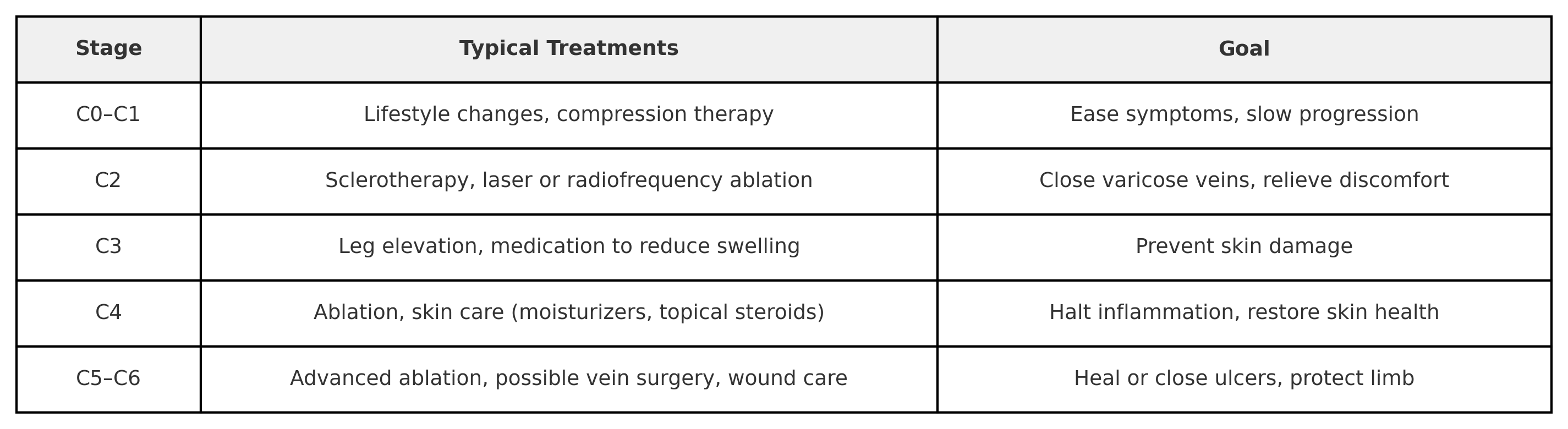
Doctors and vein specialists use the CEAP classification to grade varicose veins. As outlined by the National Library of Medicine (NIH), CEAP stands for Clinical signs, Etiology, Anatomy, and Pathophysiology; however, the “C” (clinical) stages are the part that patients need to know.
Below is a reader-friendly look at the seven clinical stages, from C0 to C6. Think of them as mile-markers on a journey, except this is a trip you want to stop as early as possible!

Stage C0–C1: The Early Warning
You may experience achy legs or mild cramps at night. Spider veins add a cosmetic concern. A vein expert typically recommends exercise, leg elevation, and compression socks to help slow the progression of vein disease. Compression therapy is a simple and effective way to improve blood flow in your legs. The Cleveland Clinic notes that compression therapy helps the vein valves push blood upward, thereby reducing swelling, easing pain, and preventing blood from pooling.
Stage C2: Classic Varicose Veins
Varicose veins are more than just unsightly and can cause leg pain, heaviness, itching, or burning. A board-certified Center for Vein Restoration specialist can perform an ultrasound to map faulty valves. Quick outpatient procedures, such as sclerotherapy or laser ablation, can seal problem veins without the need for invasive surgery of the past. These minimally invasive treatments are safe and effective options that allow you to walk the same day and return to your regular routine with minimal restrictions immediately.
Stage C3: Swelling Sets In
Swelling (edema) is more than an annoyance; it means pressure is escaping into soft tissue. If left unchecked, the skin can stretch and weaken. CVR vein experts recommend early medical care at this stage to prevent the next step, which is skin damage.
Stage C4: Skin Changes
Brownish “rust” spots (hyperpigmentation), thickened skin, or rash signal ongoing inflammation, which can become permanent. Treating venous insufficiency now involves both closing malfunctioning veins and caring for damaged skin through minimally invasive vein procedures, paired with proper skin care, to prevent further progression.
Stage C5: A Healed Ulcer
A wound that once opened and then closed again indicates that blood flow is still inadequate. Consistent compression and specialty wound care, achieved through regular check-ups with a CVR vein doctor, are crucial to maintaining the skin's integrity and preventing re-opening.
Stage C6: Active Ulcer—Time Is Tissue
An open sore near the ankle is painful and can get infected. A multidisciplinary approach will combine advanced vein treatment, wound care, and, in some cases, skin grafts.
A study published in Seminars in Interventional Radiology and reported by the NIH emphasizes that venous leg ulcers, a severe consequence of chronic venous insufficiency, require more than just local wound care for successful healing. The authors stress that addressing the underlying venous reflux or obstruction through compression therapy and procedural interventions is critical for both ulcer closure and preventing recurrence.
Without treating the root venous problem, ulcers often become chronic, costly, and disabling.
If you’re dealing with aching, cramping, swelling, or visible veins, don’t shrug it off. These are signs of chronic venous insufficiency, a progressive condition that only gets worse without proper care. The earlier you seek treatment, the easier it is to fix.
Center for Vein Restoration specializes in fast, effective vein treatments that get you back on your feet, without major surgery or downtime. Schedule an appointment today and stop vein disease in its tracks.
Waiting for veins to “get bad enough” can let minor problems turn into leg-threatening ulcers. Prompt care stops the domino effect: damaged valves → pooling blood → swelling → skin breakdown. Early, outpatient vein treatment can close failing veins, reroute blood to healthy ones, and improve quality of life.
A CVR vein specialist starts with a health history and a painless duplex ultrasound. This scan shows blood flow and pinpoints faulty valves. Duplex imaging guides your personalized treatment plan and proves insurance needs in advanced stages.
CVR accepts many insurances, including Aetna, Amerigroup, Anthem, Blue Cross/Blue Shield, Cigna, MultiPlan, Medicaid, Medicare, and more.
Questions about insurance? Call 240-965-3915 to speak with a knowledgeable Patient Services Representative.
All vein treatment procedures at Center for Vein Restoration are done in a comfortable outpatient setting, using local anesthesia. Recovery is quick, allowing you to return to your daily activities almost immediately with minimal restrictions. Parents can drive themselves to and from treatment.
These signs mean your leg veins are asking for help. A board-certified Center for Vein Restoration vein doctor can grade your disease, explain options, and tailor vein treatment so you can keep moving without fear of future ulcers.