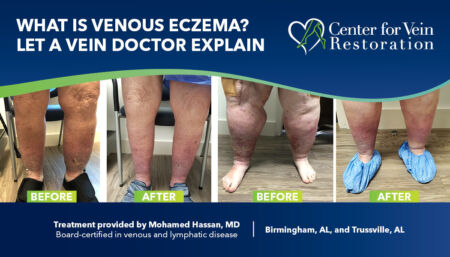
Medically reviewed by Mohamed T. Hassan, MD, DABVLM, RPVI, on May 31, 2023
The National Institutes of Health (NIH) estimates that 20 percent of people over age 70 suffer from venous eczema as part of a continuum of venous disease. Center for Vein Restoration physician Mohamed T. Hassan, MD, DABVLM, RPVI, explains how to recognize the condition and what can be done to treat it.
Venous eczema, also known as stasis dermatitis or gravitational eczema, is a condition that commonly affects the lower legs and occurs due to poor circulation in the veins. Here's some information to help you differentiate venous eczema from other pathologies, understand its treatment options, recognize misdiagnosis and mistreatment, and identify early signs of the disease that patients should be aware of.
How do I know if I have venous eczema?
Recognizing the early signs of venous eczema is vital for early intervention and preventing complications. Patients should be aware of the following symptoms:
Persistent leg swelling
Unexplained and recurrent swelling in the lower legs and ankles that worsens after prolonged standing or sitting.
Pain, itching, and discomfort
Warm temperatures often aggravate intense itching, tingling, or burning sensation in the affected areas.
Skin changes
The skin may appear dry, scaly, red, or brownish, eventually developing patches or plaques.
Ulceration
In advanced stages, open sores or venous ulcers may form, leading to pain, oozing, and potential infection.
Ways venous eczema can be misdiagnosed or mistreated
Venous eczema is often misdiagnosed or mistreated because it looks similar to other dermatological conditions, such as allergic contact dermatitis or cellulitis. Misdiagnosis is common and often leads to mistreatment, such as using topical steroids or oral antibiotics without addressing the underlying venous insufficiency. This results in incomplete relief of symptoms, worsening of the condition, or chronicity (i.e., damage to the skin that becomes difficult to cure or restore).
Common misdiagnoses include:
- Allergic reactions: Patients may be mistakenly treated for an allergic reaction without considering underlying venous insufficiency.
- Cellulitis: The similarities in clinical appearance between venous eczema and cellulitis can lead to incorrect diagnoses, resulting in unnecessary antibiotic treatment.
- Atopic dermatitis: The presence of eczematous skin lesions may lead to a misdiagnosis of atopic dermatitis, especially in individuals without apparent venous insufficiency.
Seven treatment options for venous eczema
Diagnosing and treating the root cause is the most crucial step in addressing any underlying venous insufficiency or circulatory problems. Therefore, first and foremost, patients need to get a venous duplex study to confirm venous insufficiency. If confirmed, venous ablation should be performed as the next step.
Compression therapy
Wearing compression stockings or bandages can help improve circulation and reduce swelling.
Topical treatments may be considered in acute phases
Applying corticosteroid creams or ointments can help reduce inflammation and itching.
Moisturizers
Regularly moisturizing the affected skin can help relieve dryness and prevent further irritation.
Elevating the legs
Keeping the legs elevated whenever possible helps reduce swelling and improve blood flow.
Manual lymphatic drainage and pneumatic compression pump
If the condition is associated with secondary lymphedema.
Wound Care
Proper wound care, including cleansing, debridement, and dressings, if venous ulcers develop, is crucial for healing and preventing infection.
Lifestyle Modifications
Encouraging patients to elevate their legs, exercise regularly, maintain a healthy weight, and avoid prolonged standing or sitting can significantly improve venous circulation.
Venous eczema treatment at Center for Vein Restoration
At our vein clinic, we pride ourselves on being leaders in the field of venous and lymphatic disorders. This distinction allows us to offer a comprehensive range of treatment options, making our clinic a convenient "one-stop shop" for patients seeking complete care.
From diagnostic ultrasounds to vascular interventions, skin treatments, wound care, and lymphedema management, we provide all the necessary services under one roof, eliminating the need for multiple visits to different healthcare facilities.
Meet Dr. Mohamed T. Hassan
Dr. Hassan is double board certified in venous and Lymphatic disease and in internal medicine. He is also fellowship trained in vascular interventions and has practiced medicine for over 14 years. In 2012, he decided to focus his career on diagnosing and treating venous and lymphatic disease.
Make an appointment with the leaders in vein disease
With more than 110+ locations nationwide, there’s sure to be a Center for Vein Restoration vein clinic near you!
Schedule an appointment ONLINE

 About Vein Disease
About Vein Disease
 Spider Veins
Spider Veins
 Varicose Veins
Varicose Veins
 Vein Disease Treatments
Vein Disease Treatments
 Treating Spider Veins
Treating Spider Veins
 Treating Varicose Veins
Treating Varicose Veins
 About Us
About Us
 Patient Resources
Patient Resources
 Physician Resources
Physician Resources