Leg pain and cramping commonly occur. How do you know if a blood clot is to blame?
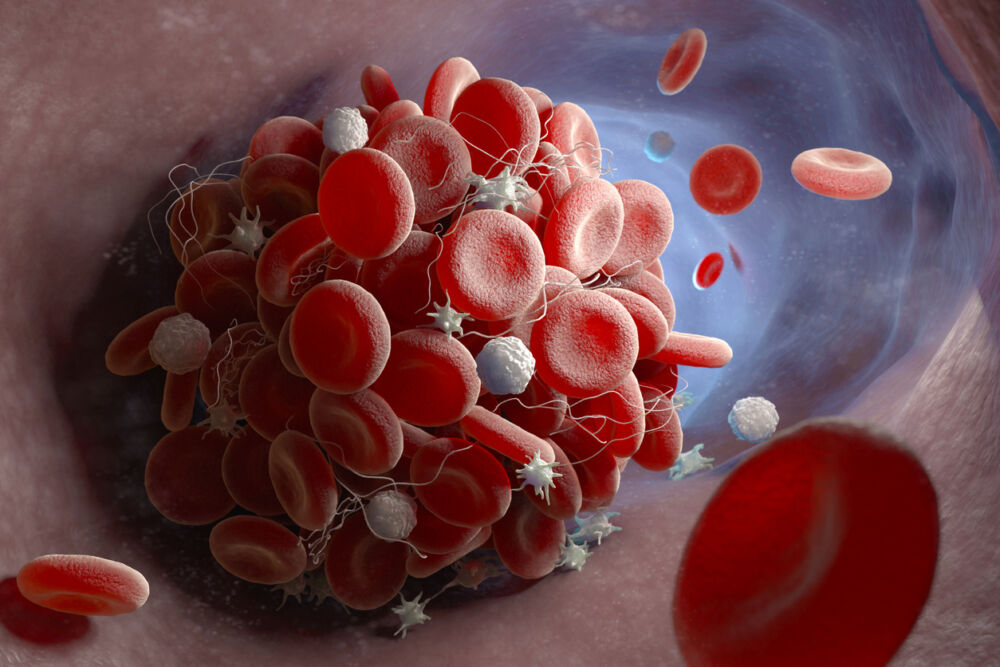
A blood clot in the leg, known as deep vein thrombosis (DVT), is a severe vascular disorder requiring immediate medical intervention to prevent a life-threatening complication. Although the clot forms in the leg, it can travel through the bloodstream and lodge itself in the lungs, causing a potentially fatal pulmonary embolism (PE).
DVT and PE affect 900,000 Americans each year. While some cases of DVT develop without noticeable signs, most people can feel a blood clot in their legs. Knowing how to identify the signs of a blood clot can help you get the quick treatment you need to prevent a PE.
What does a blood clot in the legs feel like?
Your chances of developing a blood clot rise anytime your circulation slows in the leg veins, which allows blood cells to cluster together. You create opportunities for clots to develop when you sit or stand for long periods, such as on a plane trip or in the hospital for an extended time. Other risk factors include obesity, pregnancy, smoking, advanced age, family history of clots, and hormone therapy.
Notable DVT symptoms range from pain and swelling to extreme cramping, usually only in one leg. Yet there are differences between the pain and swelling of varicose veins or a pulled muscle and DVT. One way to differentiate is feeling the skin around the affected area. When a clot forms, the skin around it may feel warm to the touch and change color to red or purple.
Cramping in the leg or a charley horse frequently accompanies a DVT. In the case of a clot, the cramp doesn’t go away when you stretch your legs. The intensity of the cramp and the swelling will increase if a clot has formed and continues to grow.
If you experience those symptoms, visit a vein specialist as soon as possible. A clot in the leg can be treated with blood thinners and other medications to break it up or slow its growth. If the clot isn’t treated, it can break free and cause a PE in the lungs, leading to shortness of breath, fever, dizziness, rapid pulse, and a bloody cough. Rush to the emergency room if you feel the signs of a PE.
How to prevent a DVT
Reducing your odds of a clot means taking good care of yourself and your veins. Here’s what you can do:
Manage your weight. Your legs already struggle against gravity to pump blood back to the heart. Adding extra pounds beyond your ideal weight only strains the veins more, resulting in blood pooling. As the blood pools, blood cells may cluster together into a clot.
Be active. When planning an exercise program, focus on workouts that engage the calf muscles, such as walking, swimming, and biking. Stronger calf muscles can support the veins in pushing blood up the heart. Even when you’re seated for long stretches, try to move around or simply flex your ankles to keep the blood circulating.
Stay hydrated. Dehydration thickens the blood, and thick blood tends to form into clots. Drink plenty of water to hydrate your body and keep your blood thin and flowing freely.
Eat a vein-healthy diet. Besides water, fruits and vegetables high in fiber and low in carbs can boost your vein health. And because these foods are low in calories, they can also help you manage your weight. Avoid foods high in sodium and fats, such as fried and processed foods. Skip the alcohol and dairy products, too.
Quit smoking. Talk to your physician about a smoking cessation program. Your veins and arteries will thank you.
Are you looking for vein care in Massachusetts?
Center for Vein Restoration (CVR) offers a full-service vein care facility in Framingham, Massachusetts. The office is led by Pamela Kim, MD, RPVI, a board-certified vascular surgeon with additional General Surgery and Vascular Interpretation certification. In addition to treating varicose veins, Dr. Kim has the expertise to treat other vascular disorders, including DVT.
Contact Dr. Kim to learn more about your treatment options or schedule your consultation appointment online today!
463 Worcester Road, Suite 205
Framingham, MA 01701

 About Vein Disease
About Vein Disease
 Spider Veins
Spider Veins
 Varicose Veins
Varicose Veins
 Vein Disease Treatments
Vein Disease Treatments
 Treating Spider Veins
Treating Spider Veins
 Treating Varicose Veins
Treating Varicose Veins
 About Us
About Us
 Patient Resources
Patient Resources
 Physician Resources
Physician Resources