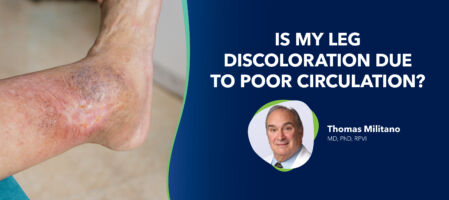
Medically reviewed by Thomas Militano, MD, PhD, RPVI, on May 29, 2025
If the skin on your lower legs has taken on a strange shade of red, brown, or purple, your leg veins might be trying to tell you something. But what?
Skin discoloration on your lower legs or ankles isn’t just a cosmetic issue; it can be a warning sign of something deeper going on with your circulation. The most common cause is chronic venous insufficiency (CVI), a condition where blood doesn’t flow properly back to your heart through the veins. That pressure can lead to dark, reddish, brown patches, swelling, and skin ulcers.

According to the Cleveland Clinic, CVI is a progressive condition, which means it worsens over time without treatment. Early signs, like skin discoloration, may seem harmless but can be the first clue that vein disease is present. Such skin is more susceptible to cellulitis than normal skin.
🎉The good news is that help is available, and most vein treatments at Center for Vein Restoration (CVR) are quick, effective, and covered by insurance.
When blood flows properly, it travels from your legs back up to your heart. But if the valves in your leg veins become weak or damaged, blood can pool in your lower legs. This condition is called venous insufficiency, and it leads to swelling, pressure, and inflammation.
Over time, the pressure from this pooled blood causes changes in the skin. You may notice:
Other possible causes of leg discoloration include:
Pro tip: If your leg discoloration lingers or is accompanied by swelling, pain, or changes in skin texture, it’s time to consult a vein specialist who can help you determine the cause.
Worried about skin changes on your legs? Trust the nation’s leader in vein care. Our experienced vein specialists at Center for Vein Restoration can pinpoint the cause and offer fast, effective treatment options performed as an outpatient and minimally invasive.

Discoloration is just one symptom of vein problems. Other signs of vein disease or venous insufficiency include:
If these symptoms sound familiar, it’s time to talk to a qualified, experienced vein specialist.
📞 Call CVR at 240-965-3915
📅 Or book online HERE
As blood pools and pressure builds in the legs, it can damage the tissues around the veins. This can lead to:
If left untreated, these skin changes can worsen and affect your quality of life.
Many people think discoloration or swelling is just part of getting older. However, vein disease is a medical condition that requires proper diagnosis and treatment.
According to a study published by the National Library of Medicine (NIH) titled Early Stages of Chronic Venous Disease: Medical Treatment Alone or in Addition to Endovenous Treatments, the condition tends to get worse over time for most people with early-stage vein disease. As it progresses, treatment becomes more involved and costly, and quality of life often goes down.
The study concludes that starting treatment early is smart, even if symptoms are mild. In the earliest stages (like when tiny spider veins first appear), conservative treatments can help reduce symptoms and improve vein function. Minimally invasive procedures may be needed for those with varicose veins.
Ignoring the signs can lead to more serious problems, including:
A board-certified Center for Restoration vein doctor will evaluate your symptoms and may use a painless ultrasound to look at the blood flow in your leg veins. This test helps identify if venous insufficiency or other vein problems may be causing your symptoms.
Treatment depends on how advanced your condition is, but may include:
1. Lifestyle Changes
2. Compression Stockings
These snug-fitting socks apply gentle pressure to the legs, helping blood move upward and reducing swelling and discomfort. These simple garments are often the first step in managing symptoms of vein disease.
3. Minimally Invasive Vein Treatments
Modern outpatient vein treatments offered at Center for Vein Restoration are quick, effective, and usually done in an hour or less with little downtime. Common procedures include:
These vein treatments help reroute blood to healthier veins and relieve symptoms.
📞 Call CVR at 240-965-3915
📅 Or book online HERE
Treating leg discoloration begins with addressing the underlying cause: poor circulation resulting from malfunctioning veins. Once the underlying vein disease is managed, the skin often improves. In some cases, your vein specialist may recommend topical creams (like hydrocortisone or moisturizers) to soothe irritated skin.
More advanced discoloration, thickening, or open sores may require wound care. If you have a venous ulcer, your vein doctor will create a care plan to help the wound heal and prevent infection.
If you’re experiencing any of the following, it’s time to visit a vein center:
Vein disease doesn’t go away on its own. But with the proper treatment, you can improve circulation, reduce symptoms, and feel more confident about your legs.
Center for Vein Restoration specializes in diagnosing and treating all types of vein problems—from early symptoms like spider veins to advanced chronic venous insufficiency. Our experienced vein doctors use state-of-the-art, minimally invasive techniques to help you feel better and get back to doing what you love.
You don’t have to live with leg pain, swelling, or skin changes. Schedule a consultation at Center for Vein Restoration today and take the first step toward healthier legs.
