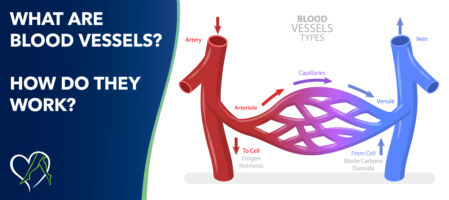
This blog explores the function of blood vessels, which are crucial components of the circulatory system, facilitating blood circulation. Blood vessels, categorized into arteries, veins, and capillaries, form the circulatory network in the body. Arteries carry oxygenated blood away from the heart, veins return deoxygenated blood, and capillaries enable nutrient exchange at the cellular level. By examining their structure and functions, we will gain insight into the pivotal role of blood vessels in sustaining life.
Blood flow through the body is a continuous and intricate process that involves the heart, lungs, and a network of blood vessels. It is essential for delivering oxygen, nutrients, hormones, and other vital substances to the body's tissues and organs and removing waste products. Understanding how blood flows through the body is fundamental to maintaining a healthy circulatory system for overall health and well-being. Learn how to check if you have poor blood circulation at home HERE.
Blood vessels are an essential part of the circulatory system. It is a network of tubes through which blood is pumped across the whole body in collaboration with the heart. This teamwork between the heart and blood vessels ensures a continuous and regulated blood flow, delivering oxygen and nutrients to every cell.
By adulthood, the body contains about 60,000 miles of blood vessels; if laid end to end, they could circle the Earth more than twice!
Per the National Library of Medicine (NIH), while blood vessels contain only smooth muscle cells, the contraction of skeletal muscle plays a vital role in the movement of blood from the periphery toward the heart in the venous system. Blood vessels include arteries, veins, and capillaries, each serving a different function:
Arteries:
Veins:
Capillaries:
Understanding these differences in the function of the different blood vessels is essential for comprehending how the circulatory system efficiently transports oxygenated and deoxygenated blood throughout the body.
Vein valves act as gatekeepers within the circulatory system, preventing the backflow of blood and ensuring that it travels in the right direction—toward the heart. Veins often work against gravity, unlike arteries, especially in the lower extremities. Valves are strategically placed throughout veins, with a higher concentration in areas where blood flow may face increased resistance.
Preventing Backflow
One of the primary functions of valves is to prevent the backward flow of blood, a phenomenon known as venous reflux or venous insufficiency. Venous reflux can lead to various health issues, including the development of varicose veins, a condition where veins become enlarged and twisted due to blood pooling.
Promoting Efficient Blood Circulation
Valves contribute to the overall efficiency of blood circulation by ensuring that blood moves steadily toward the heart. As muscles contract and relax during movement, they help propel blood through the veins. Valves facilitate this process by opening and closing in response to these muscle contractions, preventing blood from flowing in the wrong direction.
Counteracting Gravity
In areas where gravity poses a challenge to blood flow, such as the legs, valves become especially crucial. Without the assistance of valves, blood could pool in the lower extremities, leading to swelling, discomfort, and increased risk of venous issues.
Well-functioning vein valves are essential for maintaining vascular health. When valves fail to operate efficiently, conditions such as chronic venous insufficiency (CVI) may develop, potentially causing symptoms like leg pain, swelling, and skin changes.
Chronic venous insufficiency (CVI), also known as vein disease, is when the veins, particularly in the legs, become damaged and fail to return blood to the heart efficiently. This results from the malfunctioning of the one-way valves in the veins, which normally ensure that blood flows toward the heart. When these valves are impaired, blood can pool in the legs, leading to increased pressure in the leg veins and causing symptoms such as swelling, pain, and skin changes.
If left untreated, CVI can progress and lead to more serious complications, including leg ulcers. CVI is associated with risk factors such as age, family history, obesity, pregnancy, and prolonged periods of sitting or standing. Treatment for chronic venous insufficiency may include lifestyle modifications, such as leg elevation and exercise, as well as medical interventions, such as sclerotherapy, radiofrequency ablation, laser ablation, and more.
Signs that you may have chronic venous insufficiency include:
These symptoms can vary in severity, and if left untreated, CVI can lead to more severe complications such as leg ulcers or blood clots. If you are experiencing any of these symptoms, it's essential to consult a healthcare provider for an accurate diagnosis and appropriate treatment.
Minimally invasive treatment options exist to alleviate discomfort and reduce the risk of complications for problem leg veins. These treatments improve blood flow and reduce complications of vein disease such as varicose veins, leg ulcers, or deep vein thrombosis (DVT).
Seeking the expertise of a highly qualified vein care specialist is crucial for accurate diagnosis and personalized treatment plans. At Center for Vein Restoration (CVR), our board-certified physicians have extensive training in modern vein treatments and offer state-of-the-art solutions in a comfortable outpatient setting.

Each blood vessel is vital in maintaining the delicate balance required for optimal health, from hardworking veins and pulsating arteries to delicate capillaries. Embracing this knowledge empowers us to make informed choices that support the resilience and longevity of our circulatory system.
Choose wisely—choose Center for Vein Restoration as your vein health partner. Call 240-965-3915 to speak to a Patient Services Representative or schedule your consultation online at a CVR near you today.
