We spoke to Christopher M. Bulger, MD, FACS, lead physician at Center for Vein Restoration clinic in South Windsor, Connecticut, about the possible side effects of these procedures.
But before we can review the benefits and risks of varicose veins treatment, we must first understand what vein disease is—and why it is the root cause of varicose veins.
What is Vein Disease?
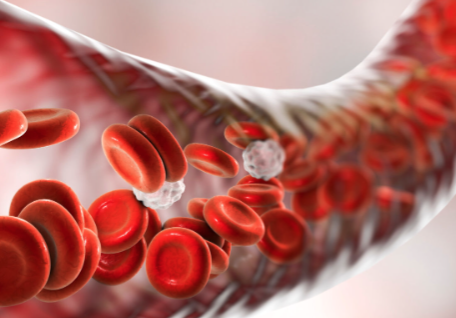
Dr. Bulger describes vein disease as “a pathology (abnormality) that affects the venous (vein) system.” He refers to the venous system is a series of “pipes or conduits that carries blood predominately back to the heart.” When this system of circulating blood back to the heart malfunctions, pain, itching, swelling, skin changes, or varicose veins can result.
Improper functioning of the vein valves in the leg can take two forms, says Dr. Bulger: obstructive and venous. Here are the differences:
Obstructive: refers to a blockage in the vein, such as a blood clot (thrombus). Deep vein thrombosis (DVT) happens when a blood clot forms in one or more of the deep veins in the body, usually in the legs. DVT can cause leg pain or swelling but also can occur with no symptoms.
Venous reflux: refers to abnormal blood flow backward in the vein. The backward flow happens when the values in the vein have failed, and gravity pulls blood “downhill,” according to Dr. Bulger.
What are the Symptoms of Vein Disease?
According to Dr. Bulger, the signs of vein disease may differ depending on the type of vein disease present: obstructive or reflux. While there is some overlap between the two types, the symptoms will vary somewhat between these two types of vein disease:
Obstructive
Suppose an obstruction such as a blood clot is causing significant blockage of the blood vessel. In that case, the person will mostly feel swelling and pain unilaterally (in one leg). However, one can also experience pain and swelling in both legs, which is “very, very serious,” says Dr. Bulger.
There are conditions in which an obstruction can progress dramatically, warns Dr. Bulger, and become a medical emergency, such as deep vein thrombosis and phlegmasia.
Reflux
Caused by faulty or weakened valves in the leg veins, blood doesn’t circulate efficiently back to the heart. Blood pools in the lower extremities, leading to symptoms such as leg pain, swelling, prominent varicose veins, itchy, aching, burning, and discomfort in one or both legs.
Venous reflux, known as chronic venous insufficiency, can progressively worsen over time, ultimately leading to skin changes and leg ulcers.
Can Vein Disease be Managed Without Treatment?
“I guess, probably,” says Dr. Bulger, adding, “but why would you?” He explains that vein disease was managed without therapy in the past when the only treatment available for reflux disease was vein stripping. Vein stripping is a difficult and damaging surgical procedure that took hours to perform under general anesthesia, required stitches to close, and was miserable to recover from.
Many patients and providers in the past understandably believed that the vein stripping procedure was so damaging that they opted for no therapy or non-invasive management, such as compression therapy alone. Dr. Bulger clarifies that compression therapy is still an effective, non-invasive management tool widely used today and required initially by many insurance carriers. Compression socks in conjunction with modern, minimally invasive techniques can safely address reflux and obstructive vein disease.
With the advent of modern, minimally invasive treatment options, Dr. Bulger recommends that a person experiencing symptoms should immediately seek treatment.
“If someone suspects that they have vein disease, they should get an opinion about it, sooner rather than later. I encourage people not to belittle their symptoms. It’s easy to say, ‘it’s not that important’ or ‘it doesn’t bother me all the time, only some of the time,’ but then it goes on for ten years...The best time to treat it is early when it starts to bother you.” - Christopher M. Bulger, MD, FACS
What Would Happen if Vein Disease Goes Untreated?
Again, the consequences of untreated vein disease differ depending on the type of vein disease one has, specifically:
Obstructive venous disorder
In the obstructive form, a person is typically treated with a blood thinner, compression, and ambulation (walking). In the past, treatment included bed rest. According to Dr. Bulger, the danger in this is that "the clot will get bigger and worse. Movement keeps blood flowing to the right places.”
If a blood clot is untreated, one could develop a condition called phlegmasia. From the Greek term phlegma, meaning inflammation, the blood flow coming out of the leg is completely blocked, limiting the blood flow coming into the leg. This condition is very painful and is a medical emergency.
The second complication of untreated obstructive vein disease is pulmonary embolism (PE). PE occurs when the blood clot breaks loose from a blood vessel in the leg and travels to a lung artery, suddenly blocking blood flow.
“Ninety-nine percent of the time, someone experiencing an obstruction to blood flow will be treated with blood thinners,” adds Dr. Bulger.
Venous reflux disorder
Venous reflux is a progressive disease, which will worsen over time. Dr. Bulger describes reflux patients as being on a bell curve. One side represents a small subset of patients whose symptoms stay the same, never getting better but not getting much worse over time.
The middle of the bell curve is where most people with varicose veins fall. For this majority, symptoms will get worse “progressively and insidiously” over several years, never getting better on its own. These people will experience “achy at the end of the day, prominent varicose veins that itch and are painful, especially when they travel. For women, they might notice painful veins during menses or in the summer veins will be hot and throb.”
On the far-right side of the bell curve falls a small sub-set of patients who experience dramatic and significant worsening of symptoms. They develop inflammatory skin changes caused by venous hypertension (high pressure within the veins). Dr. Bulger says that the tissues flooded with fluid don’t get enough oxygen, nutrients can’t flow in, and the tissue starts to scar. This results in hyperpigmentation or skin darkening that Dr. Bulger describes as a “blood tattoo.
Skin can thicken in the lower extremities above the ankle. Called lipodermatosclerosis, this condition can become permanent if not treated. Patients can also develop leg wounds that don’t heal, called ulcers.
The bottom line: Complications from untreated vein disease are painful, take a long time to heal and should be avoided through professional vein treatment.
Are There Complications of Vein Treatment?
Dr. Bulger says that there is a risk of complication with any treatment. These should again be divided into the kind of pathology and the type of treatment.
Treatment for obstructive venous disorder
Complications of DVT treatment are related to the patient’s response to the blood-thinning medication, such as an allergy or a bleeding complication. Dr. Bulger cautions that blood thinners such as XARELTO®, Coumadin, Heparin, etc., do not cause spontaneous bleeding. Rather, they make bleeding from a cut or another injury more difficult to stop.
Bleeding complications can be made worse if an extensive, invasive procedure for DVT, called thrombolysis, is required. Thrombolysis is performed in the hospital and is not as common as is the use of blood thinners.
Treatment for venous reflux
Any procedure to treat the backward blood flow comes with a small risk (about one percent) of developing a blood clot. This can happen in the vein that was treated or extend into a deeper vein, explains Dr. Bulger. Surprisingly, doctors will recommend that a superficial blood clot is treated only about half the time. The risk of being on blood thinners outweighs the risk of having the blood clot in a localized place for some clots.
Another side effect of some (not all*) vein procedures is a risk of injury to cutaneous nerves that run next to the vein being treated. This is more common in ablation procedures and happens to about ten percent of patients who have had a thermal ablation treatment to a refluxing saphenous vein. The patient may feel “an abnormal sensation or numbness in the area,” Dr. Bulger explains that a skilled provider will do their best to prevent this. Still, sometimes it’s just a matter of patient anatomy and cannot be avoided. Fortunately, this sensation does go away within three to six months.
*This risk does not apply to sclerotherapy, ultrasound-guided foam sclerotherapy, or procedures that use a medical glue to close diseased veins.
Why Ask Your Vein Physician About Complication Rates
Dr. Bulger recommends that anyone considering treatment for venous reflux ask their physician what their rate of complications is—and be skeptical not of the physicians who are open about their complication rate. Rather, be skeptical of doctors who say they have never experienced a patient complication.
Dr. Bulger warns that a physician who claims to have had no complications in their practice is either not doing enough procedures to have developed a level of expertise or are not recognizing complications that are occurring.
Why Choose Center for Vein Restoration?
The vein physicians at Center for Vein Restoration (CVR) are experts at diagnosing and treating vein disease using state-of-the-art technology in a comfortable office setting. CVR conducts over 200,000 patient interactions annually and achieves a 98 percent patient satisfaction rating.
To learn more about CVR or schedule a consultation visit centerforvein.com or phone at 240-965-3915 Schedule on YOUR schedule by booking a vein consultation online!
 About Vein Disease
About Vein Disease
 Spider Veins
Spider Veins
 Varicose Veins
Varicose Veins
 Vein Disease Treatments
Vein Disease Treatments
 Treating Spider Veins
Treating Spider Veins
 Treating Varicose Veins
Treating Varicose Veins
 About Us
About Us
 Patient Resources
Patient Resources
 Physician Resources
Physician Resources