
It is estimated that 2.5 million Americans are affected by DVT annually, and unchecked vein disease is only one risk factor. Learn the signs and symptoms, as well as options for evaluation, management, and prevention.
Sitting and being inactive can have many negative side effects to your health. One of the most insidious conditions that can result from long periods of inactivity is a Deep Vein Thrombosis, or DVT.
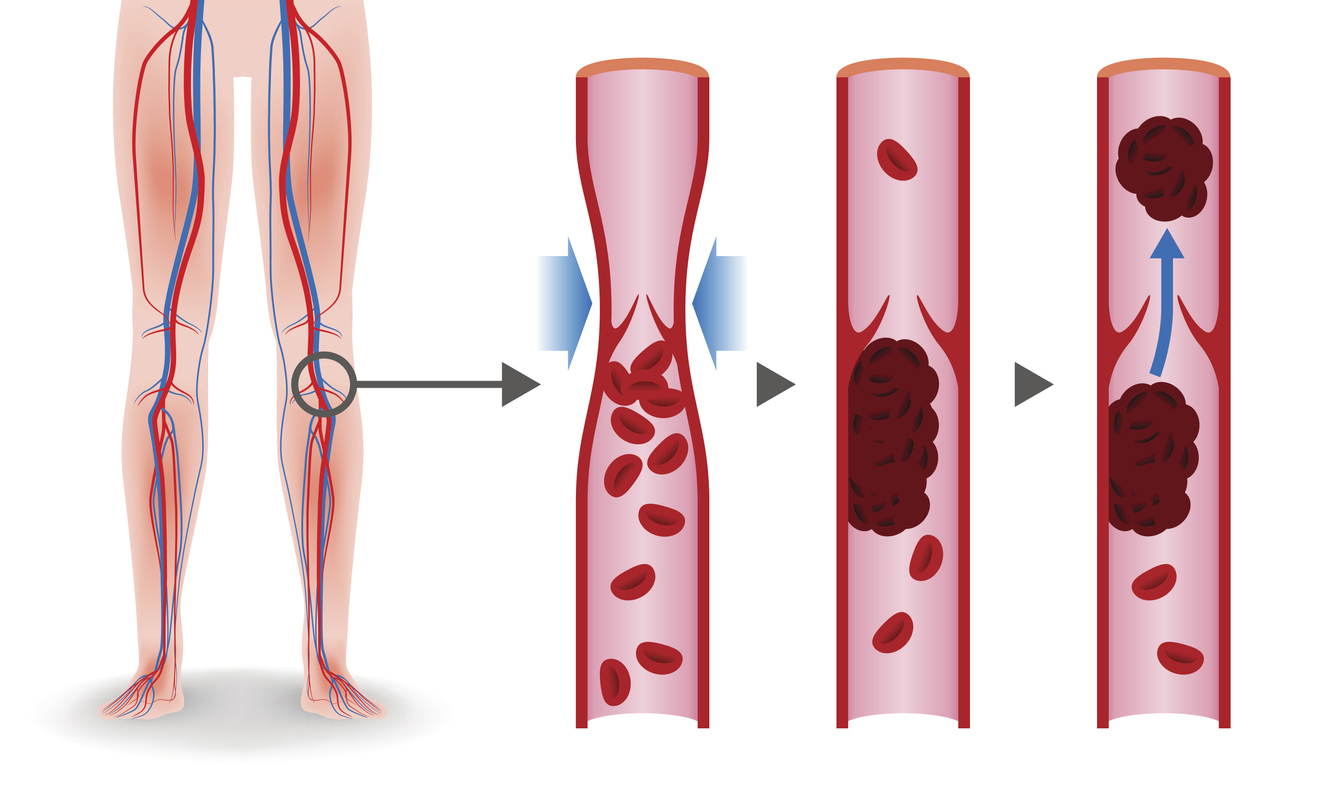
A DVT is a condition in which a blood clot (thrombus) forms in one of the deep veins in the body. After forming, the thrombus can break off and move to other parts of the body and can cause a pulmonary embolism. It is estimated 2.5 million Americans are affected by DVT each year, with over 600,000 people hospitalized annually.
By knowing the causes and risk factors associated with this condition, you can possibly avoid the hospital and safely and immediately be tested and treated in an outpatient environment.
A DVT occurs when a clot of blood forms in one or more deep veins of your legs or pelvis. The clot can be small or large. It can partially or completely block blood flow in the vein and cause a back-up of blood.
This “back-up” can lead to leg symptoms such as:
Many times, these symptoms are felt in the calf, but they can also occur in the thigh region.
A clot can also form in the superficial veins in your legs. Sometimes they start in bulging varicose veins. This can cause pain and warmth in the affected areas.

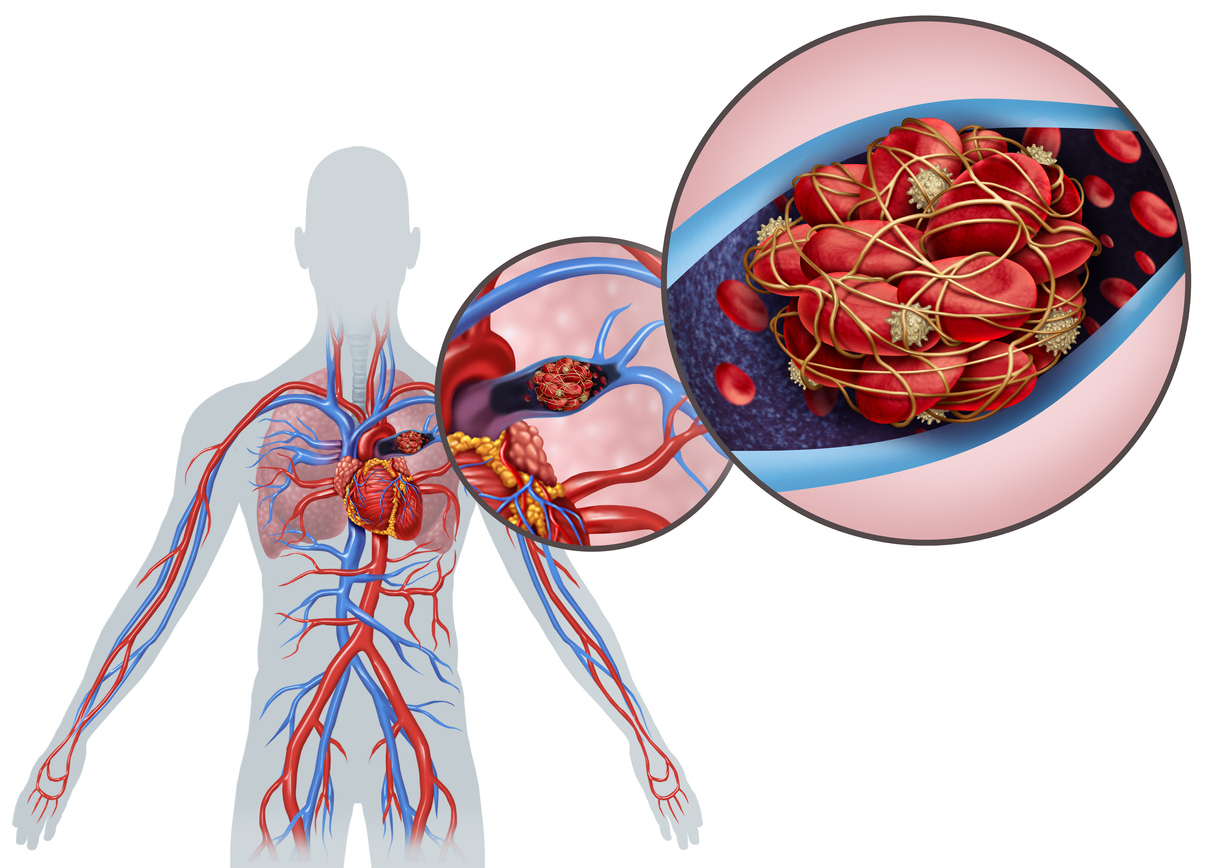
In addition to blockage of areas in the leg, a clot can also travel to or trigger a clot in the lungs. When a clot travels it is called an embolism. In the lungs, it is called a Pulmonary Embolism. A Pulmonary Embolism can be life threatening because it blocks critical blood flow in your lungs and can strain your heart.
DVT-related Pulmonary Embolisms are considered one of the most preventable causes of death. Sadly, it is estimated that 300,000 Americans die each year from Pulmonary Embolisms caused by DVTs.
The symptoms of a Pulmonary Embolism include:
An ultrasound is typically used to detect leg blood clots. Rarely, a CT scan or MRI may be needed to detect a DVT. These tests can check the size and location of the clot and also be used for monitoring for changes in a clot. Sometimes, a blood test called a D-dimer can also be helpful.
The good news is that there is treatment for blood clots. The sooner they are recognized, the sooner it can be evaluated for the need of treatment. Some smaller clots in the calf may not need treatment and can be monitored with ultrasound. Most DVT require treatment with a blood thinner. Blood thinners can come in an injection or pill form - your doctor will help you decide what is the best option for you. These are usually taken for at least three months and often longer to prevent the clot getting bigger, giving your body time to break down the clot. For some individuals, there may be a life-long need for blood thinners.
If it is not safe for you to take a blood thinner due to bleeding risk or the blood thinner is not working, you may need a filter in one of your veins, called the Inferior Vena Cava or IVC, to prevent large clots travelling to your lungs. This is called an IVC filter.
There are many factors that can increase your risk of a blood clot:
Staying active is important to reduce your risk of blood clots. If you are planning on being inactive for a long period of time, such as while travelling or when working a desk job, compression stockings can help increase circulation.
Recognizing and reducing any risk factors that you can, such as smoking or obesity, can also help. Treating conditions that increase your risk such as heart failure or venous insufficiency also reduces your risk.
In their centers across the country, Center for Vein Restoration is proud to offer a STAT DVT rule-out program to ensure patients with a suspected DVT can be evaluated in a clean, safe outpatient environment. Center for Vein Restoration’s physicians can also offer immediate intervention.
If you are worried about DVT, see your physician or vein specialist. Call 240-965-3915 to schedule with our team and find out more about your risk.
----
Seema Kumar, MD, MPP, DABVLM is the lead CVR physician in Ashburn/Leesburg CVR location. She was inspired to become a physician by her mother who practiced for many years in Cleveland, Ohio. Dr Kumar moved throughout her education and training, until she settled in Virginia in 1995, which she is now proud to call home.
Since 2007, she has practiced exclusively in the treatment and diagnosis of venous disease, it’s symptoms, and secondary conditions (such as DVT).