Learn why venous stasis dermatitis can be misidentified as cellulitis and what you can do if you have itching, discolored, thickened skin, and open sores on the lower legs.
Center for Vein Restoration (CVR) vascular specialist Mohamed T. Hassan, MD, DABVLM, RPVI, shares the recent story of his 57-year-old patient who came to CVR after ten years of chronic leg pain swelling, and progressive skin changes. Her condition had been repeatedly misdiagnosed as cellulitis. As a result, the patient was treated unsuccessfully for years with antibiotics and topical steroids.
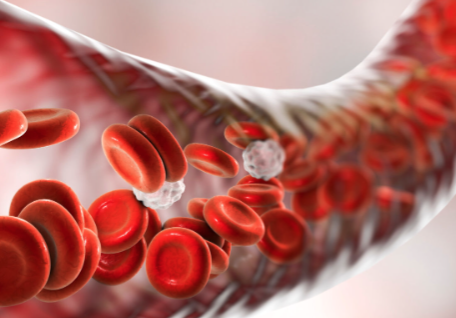
Using a venous duplex scan, Dr. Hassan correctly diagnosed the patient with chronic venous insufficiency (a condition where damaged or diseased veins valves keep blood from properly flowing out of the legs and back to the heart).
Dr. Hassan is the lead physician at CVR locations in Hoover, Alabama, and Trussville, Alabama.
What is the treatment for venous stasis dermatitis?
Once Dr. Hassan found that the actual root cause of the patient’s pain, swelling, and skin changes was malfunctioning veins, he successfully treated the patient using radiofrequency venous ablation. Radiofrequency ablation is performed as an out-patient in a comfortable CVR office setting. The procedure takes an hour or less to complete, requires only a local anesthetic, and is minimally invasive.
Dr. Hassan is happy to report that his patient is now pain-free with significant skin improvement within three months after the procedure.
Chronic venous hypertension is the most common cause of skin inflammation and stasis dermatitis in the lower extremities. I recommend that people experiencing discolored or thickened skin, swelling, itching, scaling, varicose veins, itching, or pain in both lower legs get a venous reflux study before considering antibiotics. – Dr. Mohamed T. Hassan
What is venous stasis dermatitis?
Skin changes, including inflammation caused by persistent fluid accumulation due to venous insufficiency (leaky veins) or poor circulation in the lower legs, often appear in both legs at the same time. The malfunctioning veins cause blood to pool in the lower extremities. As the fluid builds, so does the pressure in the lower legs. Eventually, bad blood products leak out of the veins and start accumulating in between the skin layers, damaging the skin.
The result changes the color of the skin to a reddish brown and can cause pain, itching, thickening and hardness, and sores that look crusty and occasionally oozes.
What is cellulitis?
Cellulitis is a bacterial skin infection that spreads rapidly and causes skin changes that usually occur in one limb. This potentially severe bacterial infection, which can be life-threatening if left untreated, enters the body through a break in the skin, possibly into deeper layers, and can spread quickly through the body. The skin can be warm and tender to the touch, and some people develop fever, chills, and blistering.
Is vein disease the cause of your skin changes? Find out! Call 240-965-3915 and speak to a Patient Services Representative to schedule a consultation today
What are the differences between cellulitis inflammation and venous stasis dermatitis?
Asymmetric pattern
Skin discoloration caused by cellulitis usually affects one leg or another area of the body. Skin discoloration caused by malfunctioning valves in the leg veins tends to be bilateral (affecting both legs).
A chronic or recurrent course
Once treated, pain, inflammation, and skin discoloration caused by cellulitis subside. Skin changes caused by venous insufficiency (vein disease) persist and worsen until treated.
Unsuccessful treatment with antibiotics and topical steroids
Cellulitis is caused by bacterial infection and is treated with prescription oral antibiotics. Inflammation caused by vein disease is not caused by infection and will not respond to antibiotics. Treatment requires closing the diseased vein, thereby sending blood circulating to nearby healthier veins.
The importance of diagnosing skin changes caused by vein disease
A patient misdiagnosed with cellulitis is not uncommon. The most common condition for which venous stasis dermatitis is mistaken is cellulitis.1
A recent study showed that 30.5 percent of patients admitted into the hospital from the emergency department of a large urban hospital with a diagnosis of lower extremity cellulitis were misdiagnosed.1.
Sadly, such misdiagnosis leads to unnecessary patient morbidity and considerable health care spending.
According to the Journal of the American Medical Association (JAMA), the national health care burden of misdiagnosed lower extremity cellulitis is significant.1 The misdiagnosis of cellulitis resulted in 84.6 percent of patients in this study not requiring hospitalization based on their ultimate diagnosis and 92.3 percent of patients receiving unnecessary antibiotics.1
Is your cellulitis not improving after treatment?
It may not be cellulitis. Schedule a venous reflux study at CVR today! Call 240-965-3915 and speak to a Patient Services Representative. Or, you may schedule online HERE. Vein care is covered by most insurances, including Medicare and Medicaid.
- Costs and Consequences Associated With Misdiagnosed Lower Extremity Cellulitis, JAMA Dermatol. 2017;153(2):141-146. doi:10.1001/jamadermatol.2016.3816

 About Vein Disease
About Vein Disease
 Spider Veins
Spider Veins
 Varicose Veins
Varicose Veins
 Vein Disease Treatments
Vein Disease Treatments
 Treating Spider Veins
Treating Spider Veins
 Treating Varicose Veins
Treating Varicose Veins
 About Us
About Us
 Patient Resources
Patient Resources
 Physician Resources
Physician Resources


