Postponed wound care during the early months of the COVID-19 pandemic leads to delayed healing for a patient visiting from Mexico.
The coronavirus slammed into the United States in January 2020, when the first confirmed case of coronavirus disease (also known as COVID-19) was reported in Washington state. By March 2020, COVID-19 was declared a national emergency in the U.S. With hospitals stretched to the limit and without a vaccine to mitigate the spread; by November of that year, the U.S. was setting new and grim records for daily cases and deaths from COVID-19.
It was during this dire and unprecedented time that Center for Vein Restoration (CVR) vein expert Kristine Cruz, MD, FACS, first met 72-year-old patient Oliva S. Dr. Cruz is the led physician at the Bronx/Pelham Bay, New York, and Bronx/ Grand Concourse, New York, CVR clinic locations.
Concerned for her welfare, Oliva’s children brought their mother to see Dr. Cruz while she was visiting New York from Mexico. Dr. Cruz reports that Oliva presented to the CVR clinic with swelling and a venous-related ulcer of the right lower leg. Oliva had been suffering from this condition for eight months and was self-treating with topical Mupirocin (a topical antibiotic).
What is a venous ulcer?
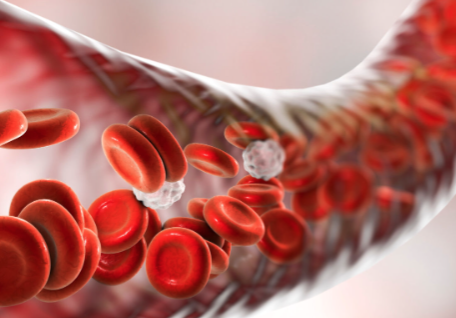
Venous ulcers are open skin sores, often on the legs. Unlike other wounds caused by cuts, punctures, or scraps, the body does not quickly start to clot and form a scab to defend the tissue from germs. Instead, because venous ulcers are caused by damaged, dysfunctional valves inside the leg veins, ulcers may not heal without appropriate treatment.
When working correctly, vein valves regulate the blood pressure inside the leg veins. Blood pressure can build in the lower extremities when valves become worn or damaged. Called venous hypertension, the increased blood pressure causes ulcers to form on the ankles.
Diagnosing a venous ulcer
During her first visit to CVR, Olivia had a venous duplex ultrasound in the office. Venous duplex ultrasound is a painless diagnostic tool that uses sound waves to look inside the body to see the veins and evaluate the blood flow within them. The test revealed venous insufficiency (vein disease) in both the deep and superficial systems of Olivia’s legs.
Because Olivia planned to return immediately to Mexico, she decided against office-based treatment in America. These procedures would have provided a permanent solution to her wound. Instead, she opted for conservative treatment of her venous ulcer using:
- Unna boot compression
- Like a cast, this gauze bandage dressing wraps around the foot, ankle, and lower leg and applies compression to the area to reduce swelling and help the wound to heal.
- EpiCeram®
- This prescription-only non-steroidal crème protects the skin from bacteria and promotes healing.
- Compression stockings
These specially designed socks apply gentle pressure to the lower leg, improving blood flow from the heart to the rest of the body and back again.
Olivia was advised to seek follow-up care upon her return to Mexico. Because all vein centers were closed due to the pandemic in Mexico, when Olivia returned to the U.S. six months later, her wound was only 10 percent healed using only conservative measures (compression stockings and EpiCeram). It was at this time that Olivia and her family decided to pursue definitive management of her vein disease with Dr. Cruz.
Treating a venous ulcer
Olivia underwent two procedures with Dr. Cruz to address her non-healing wound:
The vein physician uses heat to damage the diseased tissue during this minimally invasive office procedure, causing a scar to form, which closes the vein. Blood is then redirected to healthier veins, improving circulation. The success rate for this safe, virtually pain-free procedure is 97.3 percent.1
In Olivia’s case, Dr. Cruz performed this procedure on the patient’s right great saphenous vein, which is the largest vein of the human body. Dr. Cruz notes.
This non-surgical, minimally invasive procedure is performed in the office using ultrasound technology to guide her. The vein physician injects a medication (called a sclerosant) directly into the diseased vein with pinpoint accuracy. Patients report feeling only mild tenderness at the injection site afterward.
Dr. Cruz reports that only one week after these procedures, the patient’s ulcer was 95 percent healed!
Do you have a leg, ankle, or foot wound that won’t heal? CVR can help!
People often (incorrectly!) assume that venous insufficiency affects only the skin’s surface area (think varicose veins and spider veins) and is only a cosmetic issue. The truth is that vein disease goes much deeper into the skin of the lower limbs, causing leg ulcers that are difficult to heal. Correcting the leg veins that are the cause of the swelling and skin breakdown is an essential step toward healing.
That’s where CVR can help!
If you have dull achy pain, swelling, rashes, discolored skin around the ankle, or skin that feels tight or hot and has leathery or waxy to the touch, you must seek the care of a CVR vein expert. CVR has more than 100 vein clinics
across the United States—probably one near you! We accept all major insurances. Our physicians
are board-certified and will take the time you need to help you understand and address the root cause of your symptoms: venous insufficiency.
Call to speak to a Patient Services Representative at 240-965-3915 or schedule online HERE.
- Radiofrequency ablation of varicose veins improves venous clinical severity score despite the failure of complete closure of the saphenous vein after 1 year, Asian J Surg . 2017 Jan;40(1):48-54. doi: 10.1016/j.asjsur.2016.03.004. Epub 2016 Jul 1.

 About Vein Disease
About Vein Disease
 Spider Veins
Spider Veins
 Varicose Veins
Varicose Veins
 Vein Disease Treatments
Vein Disease Treatments
 Treating Spider Veins
Treating Spider Veins
 Treating Varicose Veins
Treating Varicose Veins
 About Us
About Us
 Patient Resources
Patient Resources
 Physician Resources
Physician Resources


